This article was originally written by Jeff Dunn for LinkedIn’s Hard Cases series, where medical professionals share the toughest challenges they’ve faced in their careers.
Code Blue Tragedy
My career took an unexpected turn in 2012 during a routine day at work. I was evaluating one of my critically ill patients in the ICU when a Code Blue was called overhead. A Code Blue means a patient in the hospital has gone into cardiac arrest, which is the most dire scenario for a patient and the providers involved. I rushed to the scene to assist the physicians and nurses already caring for a 62-year-old patient admitted for heart failure.
As I entered the room – about 60 seconds into the event – I observed the two physicians in charge blankly staring at each other. It was as if they were frozen in time and did not know the next step of treatment. The patient was not receiving chest compressions or hooked up to a defibrillator, and he was not receiving medications that could help restart the heart.
Similar to a pilot when the engine stalls or during war with adrenaline overload, the doctors were in a state of shock that unfortunately led to a lack of immediate action and ultimately this patient’s death.
Sadly, I learned first-hand that day how the choices we make as doctors, particularly in time critical events, can be the difference between life and death.
Human Error With Great Cost
Admittedly, I had made errors caring for patients and observed hundreds of mistakes that led to death or injury from the system that was supposed to improve a patient’s ailment. I went home that day, wondering how I could prevent this type of situation from happening again to any provider. I kept thinking about that patient, their family, and the providers that likely would be scarred forever. While I understood how the immediate response of healthcare providers to a Code Blue is incredible stress, anxiety, and adrenaline overload, I wanted to determine a way to manage this response more effectively.
Healthcare providers are human, which means inevitably they are going to make mistakes. One mistake can cost a patient their life or years of disability. Medical error will eventually affect you or one of your family members if we continue to be content with the status quo.
A Johns Hopkins study estimates that 250,000 patients die every year due to medical error.
Some reports state that this could be more, and my hunch from being on the frontline says it is drastically more.
Finding a Better Way
As a board certified internal medicine physician, I saw many such examples. During my years as a practicing physician, I held positions such as Chairman of Medicine and Physician Quality Leader. I had extensive conversations with hospital administrators about how we could improve care and wondered why we couldn’t perform better.
My answer to this problem was to find a way for our system to better support physicians, nurses, and EMS providers in making these time critical decisions for patients. Instead of admonishing providers, we need to assist and augment clinicians in making the best decision for patients when their life is on the line.
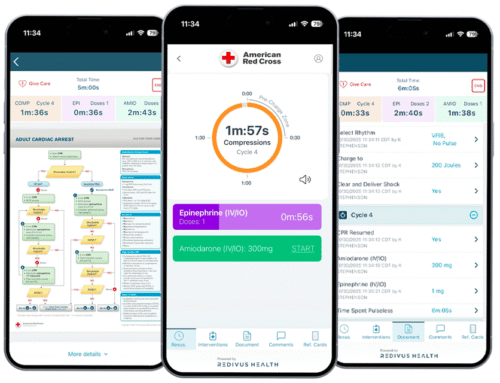
This is what led me to founding Redivus Health – a mobile technology platform that delivers healthcare providers step-by-step guidance and decision support through critical healthcare events, which are often disorganized and filled with errors.
Much like a GPS device helps drivers navigate from Point A to Point B – the Redivus Health platform helps doctors navigate through emergent events in a standardized and accessible format.
Support for Decision Making
While practicing I always wondered why there was such incredible variation in the care a patient received as it pertained to diagnosis and treatment. How could one team of doctors and nurses completely miss a diagnosis or give a patient the wrong treatment orders? This curiosity I had was not only about our hospital system but the whole U.S. healthcare system, as it relates to accuracy, efficiency, and outcomes.
Medical errors are increasingly caused by lack of standardization and consistency in our system, which is harming and killing patients. This will continue to happen unless we take some bold actions as a country to transform our healthcare system into one that is safer and more effective for patients.
I believe one place to start is offering better support for providers to ultimately better serve patients.